Watch More! Unlock the full videos with a FREE trial
Included In This Lesson
Study Tools
Access More! View the full outline and transcript with a FREE trial
Example Nursing Diagnosis for Pneumonia
- Ineffective Airway Clearance: Pneumonia can lead to airway congestion and impaired mucus clearance. This diagnosis focuses on airway management.
- Risk for Infection Spread: Pneumonia is contagious. This diagnosis emphasizes infection prevention and education on hygiene and transmission.
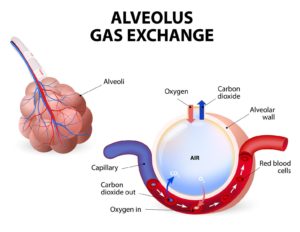
- Altered Gas Exchange: Pneumonia can result in poor oxygen exchange. This diagnosis addresses the need for oxygen support and monitoring.
Transcript
In theory, even with this, you'd have all of this extra information, but right now we're just going to talk about relevant information for a pneumonia patient. So what kind of subjective data would we have?
Here's a patient who has pneumonia. What are they telling you?
Well, they might tell you that they are short of breath and maybe they have had a fever. So their temp is high. That's objective and chills, right? Chills are subjective.
Maybe you're noticing that they're having this increased work of breathing and working really, really hard, or their respiratory rate is really high. Maybe they have a cough that you can actually hear, or possibly they reported one. Either way you're going to see sputum, and especially if they've got a bad pneumonia and it's infected, you're gonna see green sputum, which is gross.
You might hear some ronchi because, remember what's happening in pneumonia: they have a ton of fluid in their lungs, might even have an infection. So you're going to hear some ronchi. You might even hear some wheezing.
Of course this patient's gonna be exhausted. If you've ever had pneumonia, you know that you're really, really tired. If they're having really low oxygen levels, then you might actually also see some decreased LOC.
When you're gathering information on a patient, you're also gonna have bowel sounds and urine output and you're also gonna have a blood pressure and all of this other information. Part of putting together a care plan is picking out the relevant information, which is part of step two.
Step two is to analyze the information. And so we're just going to go ahead and say we've analyzed, we've determined we don't need this. This is the information we're looking at specifically for a patient with pneumonia. So we analyze the information, we gather everything and we decide what of the things I've come up with - actually a problem?
We have a patient with pneumonia. So what's their problem? Well, their problem is they have an infection in their lungs, right?
They've got all this fluid and possibly even infection. That of course puts them at risk for something like Sepsis, right? If the infection gets too bad, they can definitely get a lot worse.
Let's see, what other problems do we have while we have that ronchi and all that extra sputum. We've got all those extra secretions in the airway, right? So these are problems.
This is a significant problem for this patient. And we saw that their SpO2 was low. So what needs to be improved is their SpO2, their SpO2 level is really low and I'd like to see it higher, right?
Really we're just analyzing what's actually a problem, what's going on with this patient, what do we need to fix and what can we do.
Then we're going to establish priority. Well, listen, as easy as it is, guys, we can just go ABCs here, right?
This is an infection. This is the airway, this is oxygenation, which has to do with breathing a little bit.
Airway comes first right? So that just makes our life a whole lot easier because the ABC's always happen. Keeping their airway protected, allowing them to get the oxygen that they need, that's definitely going to be our priority.
Now we can ask our “how questions”. So for each one we're going to ask how we knew it was a problem. And this is just where we start linking our data together. So we're going to link our data, we're going to link specific data to a specific problem and then give it a specific intervention.
That's where we talk about how we're actually going to address the problem. So I have a patient, they have a ton of secretions, they have ronchi in their lungs, they have an infection in their lungs and their oxygenation is poor. So what kinds of things am I going to do?
Well, I can give them oxygen, right? I'm probably going to monitor their oxygen as well. Monitor SpO2.
I can do some sputum cultures and then give antibiotics after that, right? To try to treat that infection. Um, maybe I can encourage them to cough and deep breathe cause that's going to help them clear those secretions out. Right?
What other things can we do for those two to help open their airways? Can we do incentive spirometers right? That's going to help open up their airway. I can monitor their airway clearance. Remember, they're fatigued. So what if I would actually promote rest, because they're gonna be really tired. They're not gonna be oxygenating well. So clustering my care, promoting rest, that's going to be really helpful.
These are all little things that we can do for this patient to try to address those problems we already identified. And then how are we going to know it gets better?
Well, one of the big things we said was the problem was their airway clearance, right? So maybe we say they have a patent airway or they're able to clear their own airway. Right?
What about that oxygen level? We can say that their SpO2 increases or maybe that it's greater than 92, whatever your goal is that you want to set for your patient. And then we talked about their infection, didn't we?
They were a little bit worried about the fact that they have an infection. Um, and so maybe we could say that their signs and symptoms of infection decrease or maybe just that they don't develop sepsis. That's always a good thing, right?
These are all things you know, ronchi. So I could say their lungs are clear. There's a lot of things I could do that would give me evidence that this patient is better or that my interventions are working.
From there we're going to translate, we're going to get it into the terms that we need to use and we're going to be able to concisely communicate what the problem is for this patient. And again, here at NURSING.com, we love to use nursing concepts because we think they give you big picture priorities instead of forcing you to drill down to really, really specific issues.
Just use whatever you are required to use if there's something specific. Otherwise just come up with some top things. For this case we said the Airway was our biggest issue, didn't we? So we said I think our number one would be airway clearance, right? If a ton of sputum, a ton of secretions, they've got ronchi in their lungs, we really need to make sure their airways are open because if you give oxygen to somebody with a closed airway, it doesn't do anything for them, does it?
Speaking of oxygen, I would say that oxygenation is probably our second issue. If I have a ton of fluid in my lungs, um, I'm not really going to be able to oxygenate appropriately. So I would say that we could fairly say that's our second problem. And we know with pneumonia, oftentimes there's infection involved. So I think it's fair to say infection control would be another problem.
Here we are, we've translated it, we've said, all right, my top three priorities for this patient are airway clearance, oxygenation and infection control. So now we take those top things and the information we've gathered. And We link everything together. We're able to link our specific problem to the data, to the intervention, to the rationale, and to the expected outcome for that intervention.
Again, we said our primary problems are airway clearance, oxygenation and infection control. Let's take everything we just talked about and let's just transcribe it. We're just getting it on paper.
We're concisely communicating it in one place.
So what tells me that I have a problem with airway clearance. My patient has a cough, they have a lot of secretions. Um, and I have heard ronchi in their lungs. And again, you might've heard ronchi, you might've heard wheezes either way. If you've got airways filled with fluid and secretions, then we can't get the oxygen in it. All right?
So first thing is clear out the airway, then we give the oxygen. So what am I going to do?
We kind of talked about this already. I'm going to assess that cough. I'm going to make sure that it's getting better. I'm going to make sure it's improving. I'm going to assess those lung sounds and I'm probably gonna use an incentive spirometer. And I might even use, um, turn cough, deep breathe. I might even just encourage that cough, because it really helps them to clear those things out of their airway. I know coughing can be very uncomfortable, especially in these moments where you've been coughing and coughing and coughing. But telling your patient, Hey, if we can cough and get this stuff out, you're gonna feel a lot better.
Increased sputum means increased risk for aspiration, but also just poor oxygenation, right? So we need to be able to assess whether or not they have improved or worsened. And we can't do that if we don't assess, right?
That's why we're gonna make sure we do those assessments. And then we do things like an incentive spirometer or turn cough, deep breathe to help open up the lungs and open up the airways. Encourage coughing and clearing secretions. So expected outcome.
Again, we're still talking about airway clearance here, right? This is where we link everything. We line everything up. So expected outcomes.
My patient has a patent Airway, my patient can clear their own secretions and my lungs are clear to Auscultation, CTA, clear to auscultation. So again, we're just lining up our data and our priorities here. We've already gathered everything. Now we're just putting it on paper.
Oxygenation data, my SpO2 was low. Maybe they had a high respiratory rate or work of breathing because their body's like, oh my gosh, give me more oxygen. Right?
And that fatigue, a lot of times that fatigue is caused by Hypoxia. So what are we going to do? Well, we're going to assess that respiratory rate. We're going to watch that SpO2, we're going to promote rest.
We're going to cluster our care because of this fatigue, because again, it's just exhausting to not have enough oxygen.
Um, and then we're going to give oxygen if we need to. This PRN is as needed.
Make sure that you know what your orders are, um, so that you know what you're aiming for, right?
Get provider orders for oxygen if you don't have them. So why do we do the assessments?
Well, we need to track progress and how they're doing. We see fatigue with low oxygen like we said, so that's why we're going to promote rest and cluster care. And then of course giving supplemental oxygen is going to help keep that SpO2 up. So what are our expected outcomes?
Again, we're just linking data, right?
So I want to see that respiratory rate within normal limits. I want my patient to tell me they feel better, right? Report decreased work of breathing, report decreased fatigue and I want to see that SpO2 stay above 92 so all of these are things that are going to tell me that this is no longer a problem.
All of these things are going to tell me that this airway clearance is no longer a problem. All right, last one. Infection control. Patient had fever, chills, we saw green sputum and hey, we may even have seen an increased white blood cell count or an x-ray that was whited out with fluid in the lungs, right?
There's a lot of things that could have told us there was infection happening. So what am I going to do?
I'm going to check cultures. I always do cultures first, right? Because if I give antibiotics before I do cultures, I'm going to skew the results, right?
So cultures I'm going to give antibiotics, I might give antipyretics for that fever and I'm going to monitor their symptoms. I want to make sure that they're getting better. So again, rationales - cultures to determine the organism, antibiotics and antipyretics to treat the infection and the symptoms and monitor temp because we really want to make sure that we are controlling that fever.
So decreased signs of infection, no signs of Sepsis, cause that would be bad. That would mean they progressed and got worse. And we want to make sure we get their temp to within normal limits. Now, normal is relative, make sure you know what your targets are either for your facility or from your provider.
So just to recap on the five steps of writing an excellent nursing care plan, collect all your information, analyze that information, pick out what's relevant to that patient or those problems that you have determined.
Plan your interventions and figure out how you're going to evaluate them. So that's asking your how questions and then translate it, put it into whatever terms you need to use, transcribe it, get it on paper, use whatever form or template you prefer or you need to use. Just get it on paper. Again, remember we are just looking at this isolated pneumonia patient where pneumonia is the only problem that they have.
Remember that it might be that they have pneumonia, but they also have hypertension and they also have a pressure ulcer. And so you can look at every piece of information you have, all of your assessment data, and then determine your priorities. Airway and oxygenation is still probably gonna be at the top, but it's probably more important that I, you know, assess or you know, prevent them from getting a worsened pressure ulcer than it is that I educate them on coughing and deep breathing. Right?
So there's definitely going to be crossover priorities for this, but for this case, this was just a patient with isolated pneumonia.
I hope that was helpful.
Definitely check out the rest of the examples of nursing care plans and check out our nursing care plan library, 130 plus nursing care plan examples.
All right, guys, go out and be your best selves today and as always,
Happy Nursing!
View the FULL Transcript
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”